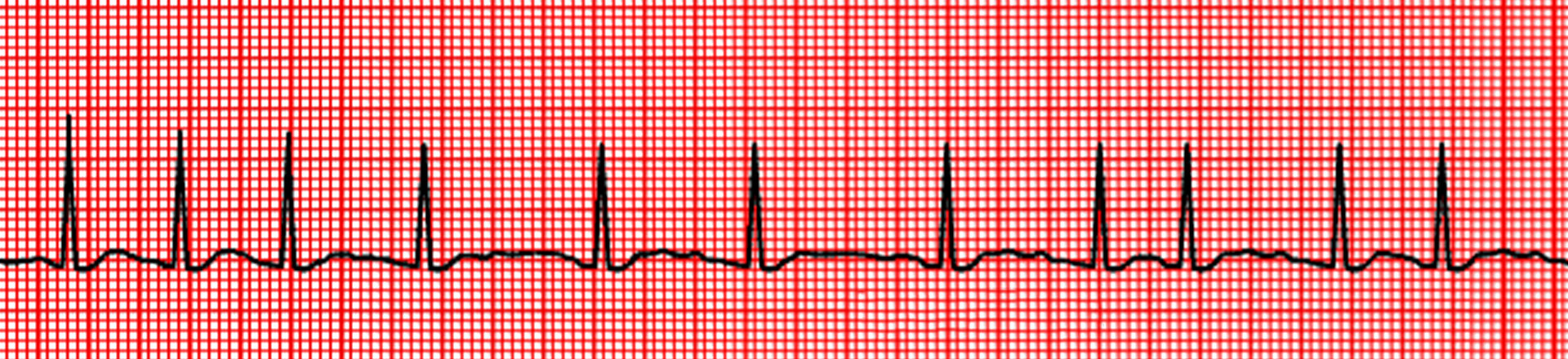
Atrial fibrillation is an abnormal rhythm of the heart. It is relatively common, affecting 2.3 million adults in the United States. The prevalence increases with age, and most people who develop A-fib are over 65 years of age.
What is Atrial Fibrillation?
Atrial fibrillation is a progressive disease and it slowly progresses from paroxysmal atrial fibrillation (intermittent) to persistent (continuous for 7 days or more) atrial fibrillation. During these stages it is still reversible and can be reverted back to normal sinus rhythm with intervention. It can progress to non-reversible stage called permanent atrial fibrillation in some people without intervention.
In atrial fibrillation (A-fib), the upper chambers of the heart (the atria) do not work correctly because of abnormal electrical activity. This means that blood is not moved out of these chambers as effectively as it should be. The blood that remains in the atria does not move as quickly as normal, which allows blood clots to form. Blood clots increase your risk of having a stroke.
Atrial Fibrillation Causes
Some people with A-fib have no obvious cause. When this occurs in people under age 65, without any associated conditions, the risk of blood clots and stroke is much lower than it is in people who are older or who have known causes of A-fib.
The risk of atrial fibrillation (A-fib) increases with age, and it typically occurs in people who have underlying heart disease. Almost any type of heart disease can increase a person's risk of A-fib, but the most common causes are:
- High blood pressure (Most common cause in US)
- Obesity
- Sleep apnea
- Heart attack
- Heart failure
- Heart valve disease, such as mitral regurgitation or mitral stenosis
- A complication of heart surgery and, less often, after other types of surgery
- Alcohol and binge drinking
- A variety of chronic lung diseases, particularly emphysema.
- Diabetes
- Chronic kidney disease.
- Family History of atrial fibrillation
- Hyperthyroidism
- Medications
Atrial Fibrillation Symptoms
Some people have no symptoms at all, while others have a variety of symptoms.
Mild symptoms can include:
- Unpleasant palpitations or irregularity of the heart beat
- Mild chest discomfort (sensation of tightness) or pain
- A sense of the heart racing
- Lightheadedness
- Mild shortness of breath and fatigue, especially with exercise
Atrial Fibrillation Symptoms
- Difficulty breathing
- Difficulty breathing with exercise or exertion
- Fainting, or near fainting, due to a reduction in blood flow to the brain
- Chest pain
- Severe fatigue
Risk of stroke- A serious complication associated with A-fib is stroke, which can lead to permanent brain damage (if the brain goes without oxygen for too long). A stroke can occur if a blood clot forms in the left atrium and a piece of the clot (called an embolus) breaks off. The embolus enters the blood circulation and can block a small blood vessel. When this happens in the brain, it causes a stroke. An embolus can also travel to the eyes, kidneys, spine, or important arteries of the arms or legs.
The risk of stroke increases with age. Other factors that increase your risk include diabetes, high blood pressure, coronary artery disease (including prior heart attack), peripheral arterial disease (PAD), heart failure, and prior stroke or embolus. Taking an anticoagulant medication reduces your risk of stroke.
When the symptoms of a stroke resolve completely within 24 hours, it is called a transient ischemic attack (TIA). Having a TIA increases your risk of having an actual stroke in the future.
Atrial Fibrillation Treatment
There are multiple components to the management of atrial fibrillation (A-fib).
Electrical cardioversion- This involves the use of an electrical current from a device called a cardioverter, delivered by paddles placed on the chest, to "reset" your heart rhythm. Urgent cardioversion is usually performed if A-fib is interfering with the heart's ability to supply blood and oxygen to vital organs.
Some people with newly diagnosed A-fib can undergo electrical or medical cardioversion (in which an antiarrhythmic drug is used to reset or restore the normal heart rhythm) immediately. However, due to the risk of stroke from blood clots lodged in the left atrium, many people are advised to delay cardioversion until they have started Cardio rhythm specialist advice with an anticoagulant.
Transesophageal echocardiogram- A procedure called a transesophageal echocardiogram (TEE) is an alternative to delaying cardioversion after starting an anticoagulant medication. It involves swallowing a thin tube, which your doctor can then view on ultrasound. This allows the doctor to see the left atrium and look for evidence of blood clots. If there is no evidence of blood clots, cardioversion can be performed without three to four weeks of anticoagulant pretreatment.
Although the TEE can avoid the need for delaying cardioversion until three to four weeks after starting the anticoagulant, it is still important to be taking an anticoagulant at the time of the cardioversion. This can be warfarin, one of the newer agents, or heparin blood thinners that are administered as an injection subcutaneously (under the skin) or intravenously (through a vein).
Although there is still a risk that cardioversion could result in a stroke even when a clot is not seen on the TEE, the risk is quite small. Following cardioversion, you will need to continue taking an anticoagulant.
Long-term physician consultation- For people with A-fib, there are two long-term Cardiologist recommendations options: rhythm control and rate control.
Rhythm control- Rhythm control involves trying to restore and maintain a normal heart rhythm (called a sinus rhythm). Approaches include cardioversion and antiarrhythmic drugs, as well as ablation. After successful conversion to normal sinus rhythm, only 20 to 30 percent of people are still in sinus rhythm after one year without antiarrhythmic drug therapy. This can be increased to 50 percent or more with the addition of an antiarrhythmic drug.
The advantages to rhythm control include improved cardiac function and, for reduced symptoms. However, rhythm control is more likely to reduce the frequency of A-fib (as opposed to eliminating it entirely). Thus, many people treated with antiarrhythmic medications continue to take an anticoagulant indefinitely.
The disadvantages of antiarrhythmic drugs are the high rate of recurrent A-fib and side effects associated with these drugs, including the development of new abnormal heart rhythms. Rarely, adverse effects of antiarrhythmic drugs can be life-threatening.
Ablation procedure for the atrial fibrillation is an option for rhythm control if medications fail or if you do not want to take medications on a long term basis due to the side effects of the medications. The ablation procedure is now become safer with development of new technology in the last 2 decades. Quality of life has improved tremendously with these ablation procedures as anti arrhythmic medications can be discontinued or reduced after the ablation procedure.
Rate control- Rate control involves trying to bring the heart rate down to a near normal level. If you are treated with rate control, you will continue to have A-fib. However, you will take a medication (a beta blocker, calcium channel blocker, or less commonly, digoxin) to slow the electrical conduction from the upper heart chambers (atria) to the lower chambers (ventricles). This keeps your heart rate in the normal range.
The major disadvantage of the rate control strategy is that it is sometimes difficult to adequately control the rate and relieve symptoms.
Non-pharmacologic treatments- There are other ways to achieve rhythm or rate control besides medication, including radiofrequency catheter ablation, and several surgical procedures.
Radiofrequency ablation- Radiofrequency ablation is a procedure that involves using heat ("radiofrequency ablation") or cold ("cryoablation") to destroy the small part of the heart that is sending abnormal electrical signals. The success of the ablation depends on the stage of atrial fibrillation at the time of ablation. If the ablation is done earlier stage like paroxysmal atrial fibrillation, the success of the procedure is upto 90%. The success of the ablation procedure decreases as the atrial fibrillation progresses.
Increasingly, this therapy is being considered an initial option in young people who have symptoms of A-fib who do not wish to take long-term medications. It is also being used increasingly in patients who have heart failure from atrial fibrillation and who are having recurrent A-fib, despite using one or more antiarrhythmic drug.
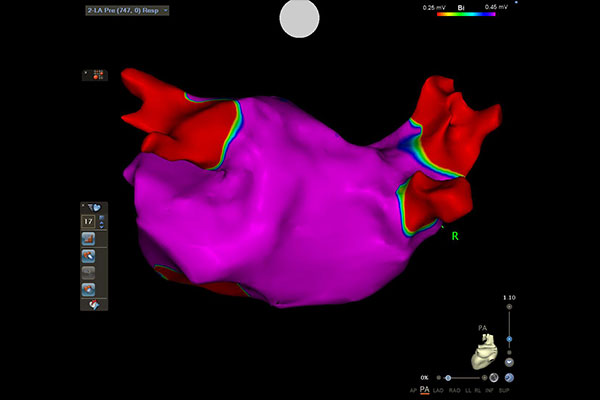
PRE AFIB PA
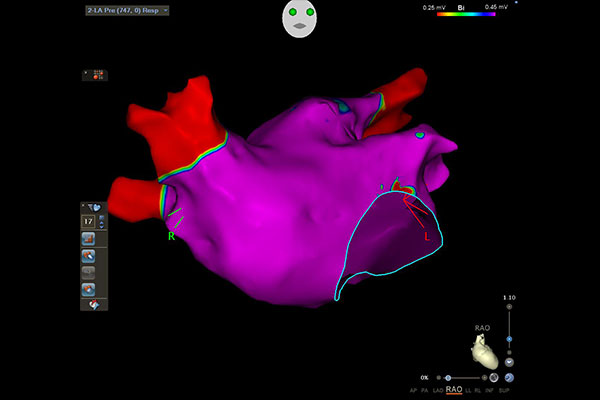
PRE AFIB RAO1
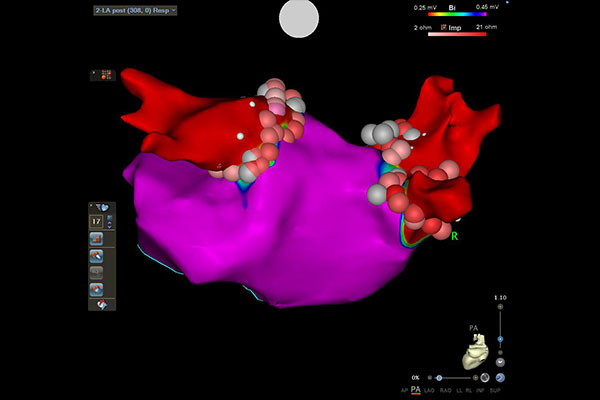
POST AF PA
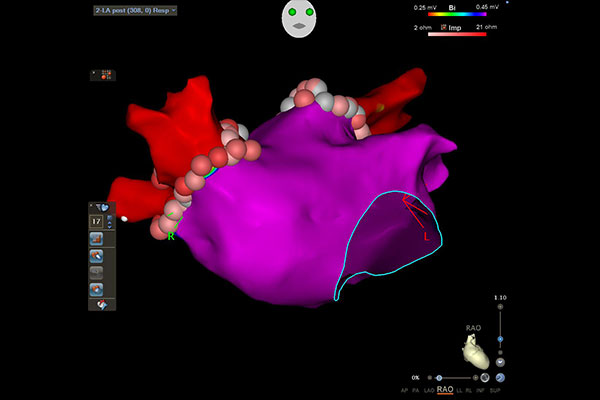
POST AFIB RAO
Surgical procedures- Surgical procedures, including the complete "maze procedure" and the less invasive alternative surgeries, may be considered in some people with A-fib, especially those who must undergo open-heart surgery for other reasons.
Stroke prevention in atrial fibrillation
The atrial fibrillation can cause
stroke and can be prevented by oral anticoagulants or left atrial appendage
closure using suture or device.
Oral anticoagulants are
- Apixiban/Eliquis
- Rivaroxban/Xarelto
- Dabigatran/Pradaxa
- Coumadin/Warfarin
Left atrial Appendage Closure
- Filter Device like watchman
- Suture closure
This video is taken from boston scientific website
Need a Doctor for Check-up?
Diagnosis, Diagnostics, and Efficient Physician Consultation Plans All healthcare plans are accepted. Visit our qualified team of physicians today!